Trichomonas vaginalis
| Trichomonas vaginalis | |
|---|---|
 |
|
| T. vaginalis phase contrast microscopy | |
| Scientific classification | |
| Domain: | Eukarya |
| Phylum: | Metamonada |
| Class: | Parabasalia |
| Order: | Trichomonadida |
| Genus: | Trichomonas |
| Species: | T. vaginalis |
| Binomial name | |
| Trichomonas vaginalis (Donné 1836) |
|
Contents |
Clinical
Mechanism of Infection
Trichomonas vaginalis, a parasitic protozoan, is the etiologic agent of trichomoniasis, and is a sexually transmitted disease.[5][2] More than 160 million people worldwide are annually infected by this protozoan.[2]Symptoms
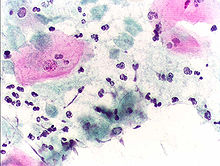
Pap smear, showing infestation by Trichomonas vaginalis. Papanicolaou stain, 400x.
Complications
Some of the complications of T. vaginalis in women include: preterm delivery, low birth weight, and increased mortality as well as predisposing to HIV infection, AIDS, and cervical cancer.[7] T. vaginalis has also been reported in the urinary tract, fallopian tubes, and pelvis and can cause pneumonia, bronchitis, and oral lesions. Condoms are effective at reducing, but not wholly preventing, transmission.[8] Ten percent of women with the infection will have a "strawberry" cervix or vagina on examination.[citation needed]Recent research also suggests a link between T. vaginalis infection in males and subsequent aggressive prostate cancer.[9]
Diagnosis
Classically, with a cervical smear, infected women have a transparent "halo" around their superficial cell nucleus. It is unreliably detected by studying a genital discharge or with a cervical smear because of their low sensitivity. T. vaginalis was traditionally diagnosed via a wet mount, in which "corkscrew" motility was observed. Currently, the most common method of diagnosis is via overnight culture,[10][11] with a sensitivity range of 75-95%.[12] Newer methods, such as rapid antigen testing and transcription-mediated amplification, have even greater sensitivity, but are not in widespread use.[12] The presence of T. vaginalis can also be diagnosed by PCR, using primers specific for GENBANK/L23861.[13][14]Treatment
Infection is treated and cured with metronidazole or tinidazole, usually as a single-dose therapy, and should be prescribed to any sexual partner(s) as well because they may be asymptomatic carriers.[15][6]Morphology
The T. vaginalis trophozoite is oval as well as flagellated, or "pear" shaped as seen on wet-mount slide. It is slightly larger than a white blood cell, measuring 9 X 7 μm. Five flagella arise near the cytostome; four of these immediately extend outside the cell together, while the fifth flagellum wraps backwards along the surface of the organism. The functionality of the fifth flagellum is not known. In addition, a conspicuous barb-like axostyle projects opposite the four-flagella bundle; the axostyle may be used for attachment to surfaces and may also cause the tissue damage noted in trichomoniasis infections.[16]While T. vaginalis does not have a cyst form, organisms can survive for up to 24 hours in urine, semen, or even water samples. It has an ability to persist on fomites with a moist surface for 1 to 2 hours.[citation needed]
Protein function
T. vaginalis has enzymes that catalyze many chemical reactions making the organism relevant to the study of protein function. T. vaginalis lacks mitochondria and other necessary enzymes and cytochromes to conduct oxidative phosphorylation. T. vaginalis obtains nutrients by transport through the cell membrane and by phagocytosis. The organism is able to maintain energy requirements by the use of a small amount of enzymes to provide energy via glycolysis of glucose to glycerol and succinate in the cytoplasm, followed by further conversion of pyruvate and malate to hydrogen and acetate in an organelle called the hydrogenosome.[17]Adherence
One of the hallmark features of Trichomonas vaginalis is the adherence factors that allow cervicovaginal epithelium colonization in women. The adherence that this organism illustrates is specific to vaginal epithelial cells (VECs) being pH, time and temperature dependent. A variety of virulence factors mediate this process some of which are the microtubules, microfilaments, adhesins (4), and cysteine proteinases. The adhesins are four trichomonad enzymes called AP65, AP51, AP33, and AP23 that mediate the interaction of the parasite to the receptor molecules on VECs.[18] Cysteine proteinases may be another virulence factor because not only do these 30 kDa proteins bind to host cell surfaces but also may degrade extracellular matrix proteins like hemoglobin, fibronectin or collagen IV.[19]Genome sequencing and statistics
The T. vaginalis genome was found to be approximately 160 megabases in size[20] – ten times larger than predicted from earlier gel-based chromosome sizing [21] (The human genome is ~3.5 gigabases by comparison.[22]) As much as two-thirds of the T. vaginalis sequence consists of repetitive and transposable elements, reflecting a massive, evolutionarily-recent expansion of the genome. The total number of predicted protein-coding genes is ~98,000, which includes ~38,000 'repeat' genes (virus-like, transposon-like, retrotransposon-like, and unclassified repeats, all with high copy number and low polymorphism). Approximately 26,000 of the protein-coding genes have been classed as 'evidence-supported' (similar either to known proteins, or to ESTs), while the remainder have no known function. These extraordinary genome statistics are likely to change downward as the genome sequence, currently very fragmented due to the difficulty of ordering repetitive DNA, is assembled into chromosomes, and as more transcription data (ESTs, microarrays) accumulate. But it appears that the gene number of the single-celled parasite T. vaginalis is, at minimum, on par with that of its host H. sapiens.In late 2007 TrichDB.org was launched as a free, public genomic data repository and retrieval service devoted to genome-scale trichomonad data. The site currently contains all of the T. vaginalis sequence project data, several EST libraries, and tools for data mining and display. TrichDB is part of the NIH/NIAID-funded EupathDB functional genomics database project.[23]


Posting Komentar